I’m preparing a series of brief lectures on aspects of coronavirus biology. Here are the first two:
Category Archives: Molecular Virology
Getting all the right pieces together to make an Influenza virus particle
Influenza virus and a few other viruses have segmented genomes. Most viruses carry their genetic information on a single piece of DNA or RNA, but influenza has 8 pieces. You can think of this as analogous to our chromosomes: we have our 20,000 genes spread out over 23 chromosomes. Each chromosome is a separate piece of very long DNA. Influenza has 8 genome segments (we don’t call them chromosomes for viruses) to encode its 11 genes.
Having a segmented genome presents a unique problem for the virus. At the end of a viral replication cycle, new virus particles must be assembled from the individual components. That usually involves assembling a capsid with the genome packaged inside, and picking up an envelope. Its complex enough to get all the components together in the right place, in the right amounts, at the right time. Influenza has the problem of needing to get 8 pieces of RNA packaged instead of just one. And it cant be any 8, it has to be one of each, otherwise the virion would not carry a complete set of instructions to successfully execute the next round of infection.
So influenza must somehow collect its 8 segments to package into the virion. When I took virology as an undergrad, I remember very clearly this problem because nobody knew how it worked. What? A major step in the replication of a major virus and we don’t know how it works? Virology suddenly seemed so exciting because there were major unanswered questions. Apparently its a hard one to answer since the details are still unknown but a strong picture is emerging from a growing body of research.
Two models have been proposed for how influenza assembles its 8 RNA segments. One, the random incorporation model, suggests that 8 randomly selected viral RNAs are packaged. This would result in most particles being defective, since the chance of selecting one of each is quite low. I’ve never been fond of this model, as it just seems too inefficient. The selective incorporation model, on the other hand, proposes that during the assembly process there is some way to select one of each genome segment.
A few studies over the last few years have advanced our understanding of the process. First, some very high quality electron microscopy revealed that the genome segments are packaged in a very specific arrangement with 7 segments in a circle surrounding 1 in the middle. Think of each segment as a dowel, bunched up lengthwise. Each segment is a different length, and each of the “dowels” in the electron micrographs appear to be different lengths, suggesting that each one is unique.

Another study used a single molecule fluorescent labeling technique to show that one and only of each of the segments is packaged into the virion. Using rather amazing microscopy, in which a single RNA molecule in a single virus particle can be detected with a fluorescent probe, they were able to show that the majority of virions carry one copy of each of the 8 segments. Several other studieshave identified unique packaging signals in the nucleic acid sequence of each genome segment. These packaging signals would serve to associate the genome segments with each other and with other components of the assembling virion.
Each one of these studies has potential problems that make them, on an individual basis, insufficient to nail the coffin shut on the random incorporation model. For example, the 7+1 arrangement is only seen in a small fraction of virions. Is it because only some have that arrangement or is it that the preparation of the samples for electron microscopy distorts some particles? This question of how influenza packages its genome serves as a terrific example of the scientific process and the necessity to generate a large body of work to figure out what may seem like a simple question. In class, we talk about designing experiments to test a hypothesis, but tend to see examples of one experiment that really nailed it. It doesn’t usually work that way. You typically need many different experiments, approaching the problem in different ways, because any single experiment could have a valid critique that weakens the conclusion. The whole body of work must be considered, and in this case the body of work appears to be supporting the selective incorporation model.
H5N1 Ferret Transmission Experiment Published
At last, one of the papers investigating H5N1 influenza transmission in ferrets has been published in the journal Nature yesterday. To recap the controversy briefly: news of experimental studies investigating transmissibility of avian H5N1 influenza hit the news this fall, igniting a fierce debate about biosecurity, “dual use” research, and the damage that censorship can have on scientific advancement. An advisory group, the NSABB, recommended partial censorship of the data, perhaps believing that redacting specific data from the publications would prevent information on how to generate a highly pathogenic mammalian transmissible virus from getting into the hands of bioterrorists or others incapable of handling such viruses safely. However, after some new data or clarification of data presented in a revised version of the submitted manuscript, the NSABB recommended publication in full.
Avian H5N1 influenza virus has caused sporadic infections in humans who have close contact with infected animals. Human-to-human transmission has not been observed. But could an H5 virus mutate or reassort, allowing human-to-human transmission?
One thing that has been lost in this whole controversy is that this study is actually a great demonstration and application of evolution. How does a virus switch to a new host and transmit efficiently between individuals? Start with a diverse population that varies in a particular trait (in this case, ability to bind the human receptor). Put it through selective pressure. This occurred in several steps: first, select for viruses that can bind the human receptor in vitro. From those that bind, select ones that can efficiently replicate in the respiratory tract of the animal. Finally, take the efficient replicators and allow for transmission. At each step of selection, mutations that naturally occur during viral replication further diversify the population resulting in variants that possess the desired property. Those variants get selected for the next experiment.
This study focused on one particular influenza virus protein, hemagglutinin (HA). HA is on the surface of the virion and is what the virus uses to attach to the host cell, the first step in viral infection. HA of human influenza viruses bind a sugar on the surface of human cells, which is slightly different from that found in the avian respiratory tract. Avian viruses, of course, bind to the form found in birds. H5 shows a strong preference for binding the avian receptor, so Karaoka et al were interested in finding out if H5 could change to recognize the human receptor, allowing more efficient transmission between mammals.
To address this, they began with a mutagenesis technique to introduce random mutations in the globular head (the receptor binding part) of HA, then used an in vitro approach to select for mutants that bound the human receptor (selection step 1). Through this process they identified three H5 variants that gained the ability to bind the human receptor while maintaining the ability to bind the avian receptor, and one that switched specificity completely to the human receptor. Several of the mutations identified in this study had already been shown in previous studies to be important in receptor specificity.
To test if the variant H5s conferred binding to human receptors in vivo, sections of human tracheal tissue were exposed to the viruses and only two were able to infect (selection step 2). This suggests the virus can infect human epithelium of the upper respiratory tract.
Next, the two remaining variants were used to infect ferrets. Both replicated in ferret respiratory tracts, but one replicated to higher levels. When they sequenced the virus that they isolated from that ferret, it was different from what they had put in: a new mutation had appeared. This new mutation presumably confers the property of better replication in the ferret respiratory tract, so it outgrew the original input virus (selection step 3).
Using this new virus (now with a total of 3 mutations in H5), transmission was tested in ferrets. Compared to the original H5, which did not transmit via aerosol, the 3-mutation variant did transmit, although between only 2 of 6 animal pairs. Again, they sequenced the virus that was present in the contact animals and found that it was different than what had gone in to the inoculated animals. Yet another mutation had appeared (selection step 4). This additional mutation appears to enhance transmission: the new virus, now with 4 mutations, transmitted more quickly and between more pairs of animals than the 3-mutation virus. Although the virus can transmit, none of the infected animals died, but they did show pathology at the site of infection.
So what does this all mean? The best model available for influenza transmission studies is ferrets. Ferrets aren’t humans, so its important to keep in mind that this is a model that helps us understand what viral or host factors are involved in aerosol transmission in these mammals, and maybe, but not necessarily, in humans. Since we don’t know what is necessary for human-to-human transmission, it is valuable to have an animal model to give us some ideas of what to look for. It can provide some good hypotheses on what mediates transmission in humans, which would then have to be further tested. Obviously, specificity for the human receptor is necessary, but the mutations identified tell us more than that. Mutations that change specificity are not sufficient for transmission. It turns out that those mutations also decrease the stability of the HA protein. The additional mutations acquired through the selection steps compensate for that, and enhance stability. So now we know that HA stability is important in influenza transmission. Between ferrets. That’s probably true for humans too, but it would need to be tested.
If you are still reading, you are obviously procrastinating, and are probably avoiding studying for your final exam. But here are some more thoughts on the controversy overall. This is a really interesting paper, with nothing particularly frightening or worrisome about it. Certainly not any more so than other papers doing similar work that were published without so much controversy. If “dual use” research needs to be regulated, it needs to be done before the work is done, not after. If the NSABB was concerned about this kind of research, why only express concern once the experiment succeeds? In my intro biology class, we read another paper, published in 2005, which was addressing the exact same question, in an almost identical way. The difference is that they failed to make a transmissible virus. If there is a concern about this kind of research, a concern that it is too risky to do these kinds of experiments, shouldn’t the alarm have been raised regardless of the outcome? It just doesn’t make sense to me why it suddenly became so concerning. If anything good has come of this controversy, it is the widespread discussion that this has stimulated on the importance of open communication of scientific data, the importance of not censoring in science. Ironically, had we all been given access to the data, like through a journal publication, it would have been apparent that there wasn’t anything to be concerned about.
Luring HIV out of its latency may be the secret to developing an effective HIV cure
Contributed by guest blogger: Steven Chan ‘12
The emergence of highly active antiretroviral therapy (HAART) in the treatment of HIV-infected individuals has certainly changed the outlook of an HIV diagnosis today, compared to what such an outlook looked like in the earliest years of the epidemic. Such a treatment regimen, if strictly adhered to, has the potential to suppress the levels of active circulating HIV in the infected individual to a level that is manageable, essentially halting the progression of the disease. It soon became clear however, that these treatments could not effectively clear the body of all HIV particles—the virus manages to stow itself away within the cellular genome of the memory CD4+ T-cells, and remain transcriptionally silent indefinitely. These latent reservoirs of HIV-infected cells prove to be undetectable for these antiretroviral therapies, since antiretroviral drugs can only target HIV-infected cells when they are replicating. And so, memory cells, which replicate infrequently, cannot be effectively targeted, making it impossible to clear HIV-infected bodies of all HIV-particles. “We’re never going to cure anybody unless we go for this latent pool,” says Robert Siliciano, the researcher at Johns Hopkins University that first identified the latent HIV memory-T cells.
A great deal of HIV-therapy research over the past decade has focused on finding a way to coax these infected cells out of their latency to make them detectable by antiretroviral drugs. The problem that has been persistently hounding researchers has been the difficulty in luring these cells out of their latency without triggering the immune system in an inflammation response that would end up doing more harm than good. David Margolis, MD, and his research team at UNC Chapel Hill, who have been working on this problem for a while now, have found success with a set of histone deacetylase inhibitors called Zolinza (vorinostat), a chemotherapeutic cancer drug that has been found to stimulate gene expression within the latent HIV-infected cells without inducing an overwhelming immune response. HDAC inhibitors accomplish this by inhibiting the activity of histone deacetylase, which removes the acetyl groups from the lysine residues in the core histones, resulting in the formation of a condensed and transcriptionally silenced chromatin. By inhibiting this activity, the core histones become less compact, and the chromatin becomes more transcriptionally active. After initial success with in vitro tests in cell cultures and in blood tissues, six HIV-positive men were recruited in a clinical trial pairing this treatment alongside consistent antiretroviral therapy. Each of the study volunteers had already been taking part in a robust antiviral regimen for an average of four years, and displayed undetectable viral loads and stable CD4+ T-cell counts. Post-exposure to Zolinza, HIV-RNA levels—a marker of viral activity—in these patients increased by an average of 4.8 times, ranging from a 1.5-fold increase in one patient to a 10.0-fold increase in another. The drug took effect in as little as 8 hours, inducing a two-fold increase in cellular and chromatin-bound histone acetylation within that time span. Increased expression made these cells susceptible to detection and eradication by the antiretroviral drugs, which proceeds just as efficiently as usual.
Margolis addresses the significance of this advancement, “This study provides first proof of concept, demonstrating disruption of latency, a significant step toward eradication.” Just how effective this drug is in teasing out the latent cells still remains to be seen—with nearly a ten-fold difference in one trial participant compared to the other, the efficacy of such a drug remains questionable. The limited sample size in this initial trial also doesn’t give us too much to go on. There are also concerns that the drug could induce some serious side effects such as blood clots in the legs and lungs, diabetes, fewer platelets and RBC count, as well as dehydration from nausea and vomiting, but at least in this trial, there were only mild adverse effects at worst. Little is known about the potential adverse effects of long-term use of the drug. Margolis et al.’s study design made use of a single dose of Vorinostat, but it is likely that repeated intermittent doses would yield the most optimal effects. “Vorinostat may not be the magic bullet, but this success shows us a new way to test drugs to target latency and suggests that we can build a path that may lead to a cure,” says Margolis. Further studies to assess Vorinostat’s safety and effectiveness, and the way it interacts with other HAART treatments, would certainly be crucial before it can be deployed as a component in future HIV treatment regimen.
Links:
Archin N, Liberty A, Kashuba A, Choudhary S, Kuruc J, Hudgens M, Kearney M, Eron J, Hazuda D, and Margolis D. “Administration of Vorinostat Disrupts HIV-1 Latency in Patients on ART,” HIV Persistence, Latency, and Eradication at 19th Conference on Retroviruses and Opportunistic Infections, March 8, 2012, http://www.retroconference.org/2012b/Abstracts/45315.htm
Contreras X, Schwenwker M, Chen CS, McCune JM, Deeks SG, Martin J, Peterlin BM. Suberoylanilide Hydroxamic Acid Reactivates HIV from Latently Infected Cells, J. Biol. Chem., January 9, 2009, http://www.jbc.org/content/284/11/6782.full
Horn T. “Pathway to a Cure: Cancer Drug Helps Purge HIV From Resting Cells,” AidsMeds, March 9, 2012, http://www.aidsmeds.com/articles/hiv_vorinostat_ cure_1667_22059.shtml
“Lymphoma Drug Wakes Up Dormant HIV,” AidsMeds, March 17, 2009, http://www.aidsmeds.com/articles/hiv_zolinza_latent_1667_16307.shtml
Steven Chan is a senior at Vassar College, majoring in Science, Technology, and Society
Zinc ionophores block the replication of nidovirus
Contributed by guest blogger: Brian Lu ’13
Zinc ions function in many different cellular processes and have been shown to play important roles in the proper folding and activity of various cellular enzymes and transcription factors, but zinc ion concentrations are kept relatively low in the cell by metallothioneins. High concentration of zinc ions and compounds that stimulate cellular import of zinc ions have been shown to inhibit the replication of various RNA viruses, including influenza virus, respiratory syncytial virus, and several picornaviruses, but details of the effects of zinc ions on nidoviruses are not well understood. Nidoviruses include major pathogens of both human and livestock, including severe acute respiratory syndrome coronavirus (SARS-CoV), the arterivirus equine arteritis virus (EAV), and porcine reproductive and respiratory syndrome virus (PRRSV). A recent study suggests that zinc ions also inhibit nidovirus replication by blocking RNA synthesis.
As high concentrations of zinc is known to inhibit cellular translation, the researchers tested if high concentrations of zinc would also inhibit viral translation. After determining the concentration of pyrithione (PT) cells will tolerate without negative effects, cells were incubated with non-toxic concentrations of PT and zinc ions. PT, functioning as an ionophore, stimulated the cellular import of zinc ions and increased the cellular concentration of zinc. The results showed a dose-dependent inhibition of viral gene expression of both SARS-CoV and EAV by the addition of PT. The inhibition of viral gene expression appears to be the result of direct inhibition of RNA-dependent RNA polymerase (RdRp) activity. The researchers also observed a dose-dependent decrease in RNA synthesis for SARS-CoV and EAV by testing the effect of zinc on the virus’s replication/transcription complex (RTC). RNA synthesis, separate from mRNA synthesis for gene expression, is an integral part of viral replication, and a decrease in RNA synthesis would imply a decrease in viral replication as well. Interestingly, the zinc ion’s effects on RNA synthesis are reversible. The addition of magnesium-saturated ethylenediaminetetraacetic acid (MgEDTA) restored RTC activity in both EAV and SARS-CoV. MgEDTA ionizes to magnesium ions and EDTA in solution, which binds to the zinc ions and prevents them from interacting with viral RTC. Adding zinc ions at different stages of RNA synthesis showed that zinc inhibits synthesis at the initiation stage for EAV but inhibits synthesis at the initiation and elongation stages for SARS-CoV.
The use of zinc ions and PT as inhibitors of nidovirus replication in cell culture can be further investigated for use as antiviral compounds, and a better understanding of the inhibition mechanism may yield future antiviral drugs against SARS and other nidovirus-related diseases. But before zinc can be used as an antiviral compound, several questions need to be answered. What is the exact mechanism for RdRp inhibition? What are the systemic effects of PT? What levels of zinc and PT would be safe for an organism? The U.S. Food and Drug Administration has approved pyrithione zinc less than 2 percent in concentration for topical use in treating dandruff, but there are no guidelines for internal uses of pyrithione zinc. It is known, however, that industrial concentrations of PT zinc is highly toxic. Additionally, in depth structural analysis and mutational studies of nidovirus RdRps is needed to determine a structural mechanism for zinc-induced inhibition of RdRp activity. Unfortunately, zinc ion binding is very fleeting and not detectable with currently available methods. As such, more sensitive methods of detecting zinc binding may be needed before the mechanism for zinc-induced inhibition of RdRp activity can be determined. Water-soluble zinc-ionophore may be better suited as the compound appears to be non-toxic even at concentrations that were effective against tumors in a mouse model. The reversible property of zinc-induced inhibition can be used in future research to gain a better understanding of nidoviral RNA synthesis. If pyrithione zinc is shown to be safe and effective in animal models, it still has to go through clinical trials before it can be used as an antiviral treatment.
Link:
http://www.plospathogens.org/article/info%3Adoi%2F10.1371%2Fjournal.ppat.1001176
Brian Lu is a junior at Vassar College, majoring in biochemistry.
Natural Resistance: How Your Genes Can Determine The Severity of Your Influenza Infection
Contributed by guest blogger: Jared Saunders ’13
Every winter, the general public frantically agonizes over influenza prevention and protection. But is the purchase of hand sanitizer in bulk and tissue boxes by the dozen really necessary? After all, many people don’t even get sick during the winter months, and some just feel a little down for a couple of days. Why do some people catch “the flu” and end up in the hospital, fighting lung infections and plowing through boxes of tissues, while others just end up with a cough or runny nose? The answer may be come down to three letters. DNA.
Recent research by Everitt et al. at the Wellcome Trust Sanger Institute (WTSI) has revealed that a single gene found in humans can determine your fate when infected with a variety of the most common strains of the influenza virus. The gene encodes the important protein referred to as IFITM3, a member of the interferon-inducible transmembrane protein family. These IFITM proteins have been shown to potently restrict the replication of a variety of pathogenic viruses, and IFITM3 has been shown to greatly alter the course of influenza infection in both mice and humans.
Brass et al. previously identified IFITM3 through a functional genetic screen that indicated it mediated resistance to influenza A, dengue virus, and West Nile virus infection in vitro. This supported the hypothesis of the WTSI group (more than 30 authors!), that IFITM proteins are critical for intrinsic resistance to these viruses, and allowed them to proceed with determining the effects of IFITM3 in vivo using mice. IFITM3 knockout mice showed severe signs of clinical illness, including massive body weight loss, rapid breathing, and piloerection (also known as “goosebumps”) when infected with low-pathogenecity strains of influenza that do not usually cause such intense symptoms. Their presentation of infection was more consistent with high-virulence strains of influenza. Contrary to the knockout mice, the wild-type mice shed significantly less of their body weight before fully recovering.
With this significant data now being collected, the group moved on to testing their hypothesis that individuals who are homozygous dominant for the IFITM3 gene develop less virulent influenza infections. They sequenced the IFITM3 gene from 53 people who were hospitalized by the H1N1 or seasonal influenza infection during 2009 to 2010 to determine if they carried the wild-type gene or one with some polymorphism. Genetic analysis of a subset of these individuals showed no evidence of hidden population structure differences with respect to a 1000 genome control group from WTSI. In the hospitalized patients, the group found significant over-representation of a specific single nucleotide polymorphism (or SNP), referred to as SNP rs12252, that has a recessive C allele substituted for a normal dominant T allele. This leads to an ineffective IFITM3 variant lacking the first 21 amino acids of the protein. This recessive C variant leads to lower IFITM3 expression in the host and consequent increased susceptibility of the host to influenza infection, and is correlated with lower levels of IFITM3 protein expression.
The group’s work has shown conclusively that IFITM3 expression can act as a barrier to influenza A virus infection both in vitro and in vivo, and that in vivo it can lower the mortality and morbidity associated with infection by a variety of human influenza viruses. Discovery of this innate resistance factor in humans may explain why encounters with a novel strain that may cause severe infections in others that do not affect you or your family.
But can the IFITM3 gene be used to help develop treatments or vaccines for future influenza strain outbreaks? Is it possible to recover this gene, if an individual has an ineffective variant, through gene therapy so as to make someone more resistant to influenza? With more research being done on the genetic aspects of disease infection, many more questions will arise, and many more answers will as well!
Links:
http://www.nature.com/nature/journal/vaop/ncurrent/full/nature10921.html
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2824905/
Jared Saunders is a junior at Vassar College, majoring in biochemistry.
Polydnavirus: Good for the Parasitic Wasp, Bad for the Host Caterpillar
Contributed by guest blogger: Jason Adler
An endoparasitoid wasp would disagree with the popular perception of viruses as malevolent. Parasitoids are organisms that spend a substantial portion of their life cycle in the host; unlike a parasite, a parasitoid usually kills or sterilizes the host. Endoparasitoid wasp oviposit into the body cavity of caterpillars. When the wasp larvae emerges, it then consumes the host as it develops.
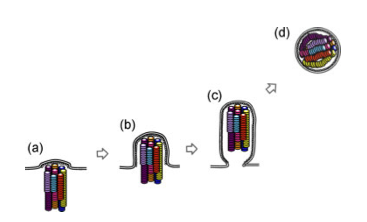
Polydnaviruses (PDV), a family of double stranded DNA insect viruses, are symbiotic to some endoparasitoid wasps. Of two PDV genera, genus Ichnovirus is specific to ichneumoid wasps and Bracovirus to braconid wasps. The PDV genome is located on host wasp chromosomes in a segmented, proviral form. However, the integrated PDV genome is not fully functional as it cannot replicate independent of the wasp and capsid proteins are non-existent. It is unknown if PDV is derived from wasp genes or if ancestral wasps integrated a beneficial PDV into their genome with resulting loss of the genes responsible for capsid formation and virus replication.
As such, PDV only replicates at specific ovarian cells during the late pupal phase, where it acquires two viral envelopes. PDV integration does not occur in the viral life cycle; instead, the viral genome is vertically transmitted to wasp offspring during meiosis. When the female wasp injects her eggs into the lepidopteran host, virions are co-injected and result in infection. Although, PDV does not replicate in the host caterpillar, it does result in immunosuppression and alters the host development (i.e. prevents metamorphosis) and metabolism to favor the parasitoid larva. The normal response of lepidopteran larvae to small foreign material is phagocytosis, but larger pathogens must be encapsulated. This is accomplished through melanization, where certain hemocytes, invertebrate immune cells found in the hemolymph, secrete melanin, which surrounds the pathogen so that anti-microbial peptides can destroy it. When immune suppressed, host hemocytes do not destroy the wasp egg by forming hemocyte nodules. Thus, PDV and the wasp share a mutualistic relationship.
Cotesia plutellae, a braconid wasp, possesses a PDV – C. plutellae bracovirus (CpBV) – and parasitizes larvae of the diamond-back moth Plutella xylotsella. Recent research has found that CpBV encodes a viral histone H4 that shares high sequence homology with histone H4 on P. xylostella, except for the last 38 residues comprising the N-terminal tail. Additionally, this viral histone H4 N-terminal tail have been observed in other Cotesia-associated PDVs. It has been suggested that the N-terminal tail is altering gene expression regulation as viral H4 histones less easily detach from DNA than host H4 histones, thereby inhibiting transcription. Is the N-terminal tail of CpBV-H4 causing immunosuppression? The researchers hypothesized that the N-terminal tail is causing the suppression of antimicrobial peptide (AMP) genes.
To examine the effects of CpBV-H4, the researchers constructed two viral recombinants: a WT CpBV-H4 and a truncated CpBV-H4 that lacks the N-terminal tail. After injection of the viral vector into the host caterpillar, RT-PCR was used to look at the expression of putative AMP genes. Although basal expression levels were unchanged, when E. coli was introduced to the host to present an immune challenge CpBV-H4 inhibited inducible expression, while truncated CpBV-H4 did not. Additionally, by counting the number of melanized black nodules on the host caterpillar after injection of E. coli and the viral vector, the researchers assessed the immune response. While the larvae show hemocyte nodule formation in response to E. coli infection, transient expression of CpBV-H4 significantly suppressed the immune response by decreasing nodule formation, while truncated CpBV-H4 had no effect. Finally, the researchers examined a possible synergistic effect of CpBV-H4 and the entomopathogenic bacterium X. nematophila. Without CpBV-H4, X. nematophila infection resulted in low mortality; however, with CpBV-H4, there was significantly increased mortality with this synergistic effect lost if CpBV-H4 was truncated.
Based on these results, the researchers concluded that the N-terminal tail appears to be responsible for immunosuppression by inhibiting inducible expression of AMP genes, possibly by altering a normal epigenetic control. CpBV-H4 containing nucleosomes may less easily detach from DNA during transcription due to the increased positive charge resulting from the increased number of lysine residues in the N-terminal tail. By introducing a virus that expresses a viral H4 histone with a N-terminal tail, the parasitoid wasp is able to suppress the host immune system. This is important as without the immune suppression, the host hemocytes would encapsulate and destroy the wasp egg.
With 157 putative genes, CpBV is likely to have more than this one mechanism to suppress host immunity. Are there other mechanisms of CpBV immune suppression? How else is the complex ecological relationship of wasp, virus, and caterpillar host mediated at the molecular level?
Link:
http://www.sciencedirect.com/science/journal/0006291X/415/2
Jason Adler is a senior at Vassar College, majoring in biology.
Discovery of an Ebola-like virus in Spain
Fans of Richard Preston’s The Hot Zone will know Ebola virus and Marburg virus as ones that causes their victims to die a horrific death, bleeding from every opening and turning organs into a bloody pulpy mess. Ebola outbreaks occur sporadically in central and west Africa, and despite extensive efforts, its still not known where the virus comes from. The best evidence is that bats carry the virus, and contact with bats or bat excrement in caves sparks the outbreaks. Ebola RNA has been detected in bats, but no one has been able to find live virus in bats.
But now a close relative of Ebola and Marburg viruses has been discovered in bats in Spain. And unlike Ebola and Marburg, which don’t cause disease in bats, it is possible that this newly identified virus is killing the bats. A recent bat die off in Spain killed several bat colonies in a little more than a week. So researchers searched for viral sequences in the bats and identified an new filovirus, and called it Lloviu virus, after the cave in which it was found. They found the same viral sequence in other caves that experienced die offs, and could not find evidence of the virus in healthy bats.
This finding is significant for several reasons. It is the first detection of a naturally occurring filovirus outside of Africa and The Philippines. The bats in Spain do not overlap with the known geographic range of Ebola and Marburg viruses so its unlikely that it would have been picked up there. There have been bat die offs across parts of western Europe, and it will be interesting to see if Lloviu virus is found at all these locations.
Also, it might be making the bats sick. The key word being might. In my class called “Microbial Wars” we have discussed Koch’s postulates and hopefully my students will recognize that these are far from fulfilled. Live virus has not yet been isolated from diseased animals, only detection of the viral genetic material. Researchers will need to demonstrate that experimental inoculation of bats with live Lloviu virus will cause the expected disease.
Cueva de Lloviu is frequented by tourists, so its possible that many people have been exposed to the virus without ever developing disease. So this is not a human health concern but it is an important discovery that may help us understand filoviruses better, especially with respect to their ecology.
Taking control of the host to spread virus laden goo
Viruses are experts at hijacking cells to replicate, manipulating the conditions in the cell to optimize viral processes. But they manipulate their hosts on a higher level too, sometimes manipulating host behaviour to increase the chances of transmission. Take rabies virus for example: the virus induces aggression, then replicates abundantly in the salivary glands and stimulates salivation. The aggressive host is driven to bite, spreading the virus to its next host.
The basis for these bahavioural changes is poorly understood, on both the viral and host ends. However an experiment published in Science recently identifies the genetic basis for host behaviour manipulation by a baculovirus that infects the gypsy moth. When a baculovirus infects its host, the host eventually dies in a gruesome death appropriately called “virus melt.” The insect is liquefied, and the gooey, virus laden liquid drips down from the remains of the host on to the leaves below. Unsuspecting insects will then eat the contaminated leaves, becoming infected themselves.
So how could a virus maximize the dissemination of said liquid? How about having the host climb to the top of the plant and stay there to die, dripping all the liquid on the leaves below? The normal behaviour of the gypsy moth is to climb up a tree and munch on leaves during the night, and hide in crevices or climb down to the soil during the day, thus avoiding predation by birds. This behaviour is regulated by a hormone, 20-hydroxyecdysone, which tells the gypsy moth when to stop feeding and move down the tree (it also regulates molting and pupation). Baculovirus infected gypsy moths, however, climb up but don’t climb back down, staying up in the tree to die.
Baculoviruses expresses a gene that deactivates 20-hydroxyecdysone and prevents the infected host from leaving its “feeding state” and descending the tree. When researchers deleted the gene from the virus, the infected gypsy moths displayed normal behaviour.
I’d love to see a transmission experiment to see if the presence of this gene really helps with transmission to the next host.
(Also discussed on TWiV)
Broad Spectrum Antiviral is an Effective Inhibitor of Viruses but Not Media Hype
There have been a few important successes in antiviral drug development, but for the most part it is extremely difficult to find drugs to treat viral infections. Viruses are highly effective hijackers of cellular processes, and since drugs that target cellular processes are likely to be toxic, that leaves only a few potential virus specific targets. Further, because of the diversity of viruses most antiviral drugs are very specific for their target virus and are not effective against others. The holy grail of antiviral drugs would be something that inhibits replication of many viruses – a broad spectrum antiviral.
A new paper in PLOS One describes a creative approach to the problem of broadly targeting viral infections. The approach uses a recombinant protein that combines the properties of two natural antiviral response pathways in the cell. Almost all viruses generate long double stranded RNA (dsRNA) at some point in their replication cycle. But long dsRNA is not found in normal, healthy cells. So the presence of dsRNA triggers a response in the cell that shuts down gene expression, which can effectively shut down viral replication. Another response is apoptosis: an infected cell can trigger a cellular suicide pathway, destroying the infected cell and the virus along with it. In this new study, researchers fused parts of proteins from key mediators of both pathways to generate a new protein called DRACO that triggers apoptosis when it binds to dsRNA.
In cell culture, DRACOs induce apoptosis in cells only when dsRNA is present. The study goes on to test whether DRACOs can protect cells from infection. Cells pre-treated with DRACOs survive viral infection, while untreated cells don’t. And it protects against a large variety of different viruses; viruses from 7 different families were tested and DRACOs appear to be effective against all of them. But for an antiviral to be useful it has to also work in vivo, and DRACOs show some promise here too. 60-70% of mice pre-treated with DRACOs survive influenza virus challenge, while only 10% of untreated mice survive.
The results of this study are exciting and show promise but we must be cautious about over-extending the findings. It is a long and challenging process to go from an early stage development like this one to a clinically useful anti-viral drug. There will be some very significant hurdles to overcome to develop this further. In all the experiments, the cells (or animals) are pre-treated with DRACOs, but its not known if there is any post-exposure protection. The animal studies show that interperitoneal injection can protect animals, but the distribution of the drug in different tissues varies and in some tissues disappears before 24 hours, which could be a problem if it can’t reach the required concentrations in the target tissues. Also, being a protein, there will be challenges for effective delivery (since interperitoneal injection is not likely to be a favored route!). Many years of further testing, development, and clinical trials (if it gets that far) are needed. Despite the many challenges that lay ahead for further development of this broad spectrum anti-viral, it appears promising and worth pursuing.
As usual though, news reports describing this as a major breakthrough have missed the point that this is an interesting new development but that it is very much in its infancy. Since nearly every discovery is hailed as a breakthrough, the public gets a distorted idea of the way science proceeds. Media reports have also been misleading, including promoting it as a potential treatment for HIV or Hepatitis, which weren’t even among the viruses tested, or touting it as a possible cure for nearly all viral infections. Slow down a little, folks. There is a long way to go before those claims can be made. Perhaps someone can develop a treatment for the disease that makes headline writers distort information.

